Polysomnographic validation of the Sleeptracker-AI® solution in estimating sleep architecture and obstructive sleep apnea in adults
Polysomnographic validation of the Sleeptracker-AI® solution in estimating sleep architecture and obstructive sleep apnea in adults, in collaboration with Stanford Sleep Medicine, as presented by Dr. Clete Kushida at the 2022 Sleep World Congress in Rome (Italy).
Featured in Sleep Medicine
Volume 96, August 2022, Pages 20-27
Highlights
- An under-mattress sleep monitoring device (Sleeptracker-AI Monitor) was compared with polysomnography (PSG).
- Sleeptracker-AI Monitor estimated comparable sleep measures and had high agreement in sleep stage classification with PSG.
- Sleeptracker-AI Monitor had high accuracy in estimating obstructive sleep apnea.
Reference: Ding, F., Cotton-Clay, A., Fava, L., Easwar, V., Kinsolving, A., Kahn, P., Rama, A., & Kushida, C. (2022). Polysomnographic validation of an under-mattress monitoring device in estimating sleep architecture and obstructive sleep apnea in adults.Sleep medicine, 96, 20-27.
Stanford validated and Peer-Reviewed
Read the entire publication at Science Direct:
https://www.sciencedirect.com/science/article/pii/S1389945722001368
A two-year+ study on the COVID-19 effect on sleep
The COVID-19 pandemic has affected sleep in multiple ways. Technological advances www.sleeptracker.com in-home sleep monitoring has provided the opportunity to analyze sleep-wake patterns on a scale much larger than previously imaginable. This study compares the estimated sleep-wake patterns in the time before and after the start of the pandemic in a large U.S. sample.
Sleep parameters [estimated total sleep time (TST), bedtime (BT), and morning rise time (RT)] were analyzed. The device passively monitors sleep using piezo-electric sensors that register the forces exerted through the mattress by features such as the individual's motion, respiration, heartbeats, and snoring vibrations. The de-identified data obtained from the devices were analyzed, following review and exemption of the study (#57681) from the Stanford University IRB. Data from the calendar years 2019 and 2020, from 62,152 individuals with 20,255,441 recorded nights, were available. Individuals who had at least 300 nights of sleep each year were included in the analytic dataset, with Sunday nights through Thursday nights analyzed since sleep on weekend nights was expected to have more variability.
Irregular sleep-wake schedules and the impact on health
Cardiovascular disease, increased blood pressure, stroke, and insulin resistance are associated with Irregular sleep-wake schedules
This very large study is the first extensive home study with more than 4 million nights of accurately recorded sleep patterns.
Interestingly, this study finds a clear age-dependent trend, with older age corresponding to more regular sleep-wake schedules.
The importance of REM-rebound
REM sleep is an essential component of sleep. "REM-rebound” is an evolutionary mechanism to help us get some of that precious REM-sleep back.
Most of us are typically sleep-deprived during weekdays and attempt to recover our lost sleep on the weekends. This first-of-a-kind, extensive study of more than 6.8 million nights of sleep as per Sleeptracker-AI explores the weekly rapid-eye-movement (REM) sleep deprivation-recovery cycle. This study validates the repetitive REM sleep deprivation-recovery cycle. Individuals are, on average, partially sleep-deprived starting Sunday night, which leads to a progressive REM sleep rebound that transitions into a REM recovery cycle on Friday and Saturday nights.
Background: After early research connected rapid eye movement with dreaming and established that it made up about 20% of normal human sleep, experimenters started depriving test subjects of only REM sleep to test its unique importance. Whenever a subject's electroencephalogram and eye movements indicated the beginning of REM sleep, the experimenter would thoroughly wake them for several minutes. As this "dream deprivation" continued, the tendency to initiate REM increased and the subjects were woken up more and more times each night. As a result, the subjects became irritable, anxious, and hungry, and several left the study early. Finally, after five nights, the remaining issues were allowed to sleep undisturbed and showed a significant increase in the percentage of sleep devoted to REM: from an average of 19.4% to an average of 26.6%. These effects were significant in comparison with a control group woken up on an equal number of occasions each night, at random times.
Further reading:
What is REM sleep?
https://www.sleepassociation.org/about-sleep/stages-of-sleep/rem-sleep/
The importance of REM rebound and CPAP compliance
https://www.sciencedirect.com/science/article/abs/pii/S1389945712001864
How bed-partners impact each other's sleep quality
A joint study between Stanford Sleep Medicine and Fullpower-AI.
Sharing the bed with a partner is common among adults and is likely to impact sleep in multiple ways. However, gold standard polysomnograms are performed without a bed partner, and objective data on co-sleeping couples is scarce.
This large study of over 5,000 users investigates the effects of a bed partner's presence on objective sleep parameters.
This detailed, science-based study suggests that when the bed partner is absent, an individual's sleep architecture shows, on average, a higher sleep efficiency, with less micro-awake time and total sleep, more minutes spent in deep and REM sleep, and less in light sleep. This suggests a less interrupted night, perhaps due to fewer disruptions from the partner, where the individual has enough continuity in their sleep to transition to deeper stages. Just like with pets sharing our bed, it's challenging to quantify the counter-balancing positive emotional impact of having a bed partner.
Further reading:
The effects of sleep continuity disruption on positive mood and sleep architecture in healthy adults
https://academic.oup.com/sleep/article/38/11/1735/2662282
Snoring and sleep architecture
https://www.atsjournals.org/doi/abs/10.1164/ajrccm/143.1.92
Reference: Zitser, J., Cotton-Clay, A., Baron, S., Easwar, V., Kinsolving, A., Kahn, P., & Kushida, C. (2022). 0353 Estimated Sleep-Wake Patterns Obtained from a Large US Sample by Home-Based Under-Mattress Monitoring Devices. Sleep, 45(Supplement_1), A159-A159.
https://academic.oup.com/sleep/article/45/Supplement_1/A159/6592308
Evaluation of Sleep-Related Respiratory Events
In an extensive longer-term study, the data shows that more than 14% show moderate to severe apnea (AHI>15) as presented at the Athens Greece sleep conference, September 2022.
This is the first known large-scale continuous Sleep Apnea study. Sleep Apnea is a potentially serious sleep disorder. It causes breathing to stop and repeatedly start during sleep. Studies have found a direct correlation between High Blood Pressure, Diabetes, Stroke, heart attack, and Apnea. In a large study of over 75,000+ sleepers, over 14 million nights of sleep. The data shows that more than 14% experienced serious sleep apnea at least one night a week. There are effective therapies for apnea. The diagnosis must come first. There are several types of sleep apnea, but the most common is obstructive sleep apnea. This type of apnea occurs when your throat muscles intermittently relax and block your airway during sleep. A noticeable sign of obstructive sleep apnea is snoring. Population studies have estimated the prevalence of sleep-related respiratory events characteristic of obstructive sleep apnea (OSA) and reported night-to-night variability in OSA severity. Still, these have been constrained by the inability to obtain continuous nightly data on a large scale. The current study is the largest to date for evaluating these events' prevalence and night-to-night variability. The de-identified data from 2021-04-01 to 2022-03-31, in 76,769 individuals with 14,296,394 recorded nights. Individuals with at least 300 nights of recordings were included in the analytic dataset.
Sleep Duration Effect on Heart and Respiratory Rate
This new, large long-term study by Stanford and Fullpower-AI may show that we should strive to sleep between 6 and 9 hours. Not less and probably not more. As presented at the Athens, Greece, 2022 Sleep summit two weeks ago.
Intuitively sleep deprivation is unhealthy. This very large study shows that sleeping too much, hence 9 hours or more, may not be beneficial. This study looks at the length of actual sleep as opposed to the time spent in bed. This correlation could mean that 6.5 to 8 hours of sleep may be optimal for health. That's because resting heart and respiration rate are generally considered signposts of wellness.
Sleep data from 76,769 users, with 14,296,394 total recorded nights from 2021-04-01 to 2022-03-31; only subjects with at least 300 nights of recordings during the period were included. In total 18,252 individuals (40% female, 13% unspecified gender, mean age 49) with 5,846,745 recorded nights met this inclusion criterion. Estimated total sleep time (TST) was categorized as: <5 hours, 5-6 hours, 6-7 hours, 7-8 hours, 8-9 hours, and >=9 hours. Normalized Heart Rate (HR) and Respiration Rate (RR) for a recording were taken to be the mean HR and RR for that recording as a percentage of the average over all recordings for that subject. Excess HR and RR for a recording were taken to be the excess/deficit of the normalized HR and RR over 100%. Subjects had lower HR and RR than average on nights when they slept 7-8 hours. Interestingly, their HR was higher than average on nights when they slept <6 hours or >=9 hours.
Notably, the American Academy of Sleep Medicine recommends >=7 hours of sleep without an upper limit. Furthermore, these findings may inform on the relationship between extreme sleep duration as a risk factor for cardiovascular events.
Here is an article from Mayo Clinic about Cognitive Behavioral Therapy for sleep.
The number of nights needed for OSA detection
Obstructive Sleep Apnea (OSA) is a sleep disorder that occurs when breathing is repeatedly interrupted during sleep. It's often caused by a blockage in the airway, leading to loud snoring, choking, and gasping during sleep. OSA can cause daytime sleepiness, fatigue, and other health problems, and getting a proper diagnosis and treatment is important. OSA is typically diagnosed through a sleep study, which can be conducted in a sleep lab or at home. During a sleep study, various measurements are taken to evaluate your sleep, including breathing patterns, oxygen levels, and brain activity.
Clinical sleep studies typically rely on one night for OSA detection and diagnosis. However, uncertainty exists regarding the degree of AHI stability across different nights. Population studies collecting continuous nightly data on a large scale enable the detection of night-to-night variability in OSA severity; this study is the largest to date for evaluating the number of nights to achieve high sensitivity/specificity for OSA detection. This extensive study led by Dr. Clete Kushida of Stanford Sleep Medicine builds on 96,228 individuals with 19,148,323 recorded nights.
Reference: Kushida, C., Cotton-Clay, A., Fava, L., Easwar, V., Kinsolving, A., & Kahn, P. (2023). 0502 Number of Nights to Achieve High Sensitivity/Specificity for Detecting OSA Using a Large US Sample by Home Under-Mattress Devices. Sleep, 46(Supplement_1), A222-A223.
https://academic.oup.com/sleep/article/46/Supplement_1/A222/7182096
Reference: Kushida, C., Cotton-Clay, A., Baron, S., Fava, L., Easwar, V., Kinsolving, A., & Kahn, P. (2023). Detection and Prevalence of OSA in Men and Women using a Continuous Large US Sample by Home Under-Mattress Devices. CHEST, 164(4), A6286-A6287.
https://journal.chestnet.org/article/S0012-3692(23)05084-5/fulltext
New very large Sleeptracker-AI® Sleep Study in partnership with Stanford Sleep Medicine
Fullpower-AI®, in a very large-scale sleep study, presented new findings at the World Sleep Congress in Brazil. This study shows the first large-scale quantification of declines in deep and REM sleep with age. Practically speaking, this is one of the reasons why maintaining enough deep sleep can be vital for overall health.
With the Sleeptracker-AI® platform, which leverages deep learning and generative AI, and in collaboration with Stanford Sleep Medicine, Fullpower-AI® studied 24,850,420 nights of sleep and presented findings at the World Sleep Congress in Brazil.
While it's recommended that adults sleep at least seven hours per night, this large-scale study provides new insights into how sleep duration and architecture vary with age. Most people undergo 75-80% of their sleep in NREM (non-REM sleep) and the rest in REM. The study shows that the middle-aged population tends to sleep less, and as people age, there's a significant decrease in deep sleep consistent across ages. In REM sleep, steep declines begin in late middle age. Notably, those with sleep apnea experience an even more significant decrease in deep sleep regardless of age, emphasizing the impact of sleep apnea on overall health and the need for remediation.
What This All Means for Improved Health
Understanding sleep patterns and architecture is crucial for overall health. These findings emphasize the importance of adequate sleep quality, especially as one ages. The decline in deep sleep, particularly for those with sleep apnea, indicates the need for proper diagnosis and treatment. By addressing these sleep disturbances, individuals can work towards achieving better health and reducing risks associated with sleep deficiencies.
Fullpower-AI® New Findings in Major Apnea Study
Dr. Clete Kushida of Stanford presents a new extensive study, collaborating with Stanford Sleep Medicine and Fullpower-AI®, at the World Sleep Congress 2023 in Rio de Janeiro.
The study shows the health benefits of consistent CPAP use by people with apnea in 720 female and male patients, using 58,000+ nights of sleep monitored in high fidelity with Sleeptracker-AI® in their homes. Sleeptracker-AI® can monitor sleep during CPAP usage, including when it is not used. The findings show significant decreases in breathing anomalies when CPAP is used.
Sleeptracker-AI® uses AI to analyze sleep data anonymously collected to help identify different sleep stages, detect sleep disorders, and provide users with personalized sleep recommendations. It closely matches in-the-home, contactless, gold-standard PSG sleep analysis in real-world settings with machine and deep learning models and statistical inference techniques while carefully considering bias and other ethical issues. Its methodologies include deep, supervised, self-supervised, and reinforcement learning techniques. To continually generate training data, multiple clinical PSG sleep labs are in operation.
Whether one has Obstructive Sleep Apnea (OSA) or Central Sleep Apnea, the data shows that consistent use of a CPAP can make a difference in sleep quality and overall health.
Here's why:
OSA: With OSA, the airway gets blocked during sleep, causing breathing interruptions and sleep disturbances. A CPAP machine delivers a continuous pressurized airflow, keeping the airway open and ensuring stable oxygenation (SpO2).
Central Apnea: For those dealing with Central Sleep Apnea (about 10% of the population diagnosed with apnea), it's neurological, and the brain's signal to breathe seems to be temporarily disrupted. A CPAP with adaptive settings can help stabilize breathing patterns.
Sleeptracker-AI® studies also show the benefits of consistent CPAP use:
- Improved sleep quality: wake up feeling refreshed and energized.
- Increased alertness: better concentration and daytime alertness.
- Reduced health risks: Lowered risk of heart disease, stroke, and other sleep apnea-related health issues.
- Enhanced mood and mental outlook.
The data clearly shows that with apnea, the key is a consistent use of the CPAP.
Fullpower-AI® NEW Very Large Sleep Apnea Study
I am excited to share groundbreaking research on Obstructive Sleep Apnea (OSA) detection and prevalence, presented at the Seville Sleep Conference! Our Sleeptracker.ai platform, in collaboration with Stanford Sleep Medicine and UCSF, has conducted one of the most extensive studies in this field.
Key Findings:
- Analyzed 17,173,525 nights of sleep data from 52,637 participants
- Revealed limitations of single-night OSA assessments
- Discovered higher OSA prevalence in women ≥50 years compared to younger women
Why This Matters:
Continuous Monitoring: Our Sleeptracker.ai enables non-invasive, nightly sleep tracking, providing a more comprehensive view of sleep health.
Improved Detection: Maximum AHI across 3 nights shows high sensitivity (≥95%) for detecting moderate to severe OSA.
Gender and Age Insights: Women over 50 show a greater increase in OSA odds compared to men, potentially linked to menopausal factors.
Personalized Care: Identifying OSA severity fluctuations over time allows for more tailored treatment approaches.
Early detection and management of OSA can significantly improve quality of life and reduce associated health risks. Our research demonstrates the power of continuous sleep monitoring in revolutionizing sleep health assessment and care.
We are proud of our team and grateful for our collaborators in pushing the boundaries of sleep science! Sleeptracker.com
Estimated Sleep-Wake Patterns Obtained From a Large U.S. Sample Using a Home-Based Under-Mattress Sleep-Monitoring Device

Featured in the Journal of Sleep Medicine
Volume 21(3), December 31, 2024
Highlights
- Recordings were obtained using an under-mattress sleep monitoring device (Sleeptracker-AI Monitor).
- Sleeptracker-AI Monitor estimated comparable sleep measures and had high agreement in sleep stage classification with PSG.
Obstructive Sleep Apnea Detection and Prevalence in Men and Women Using a Continuous Large U.S. Sample by Home Under-Mattress Devices
Featured in
Sleep Medicine Online, September 16 2025
Highlights
- The prevalence of OSA is influenced by gender and age.
- Single-night sleep study may inaccurately classify OSA severity due to night-to-night variation.
- Home-based continuous sleep monitoring devices have the potential to enhance OSA diagnosis and address night-to-night variability.
- Sleeptracker-AI Monitor exhibits high sensitivity and specificity in diagnosing OSA during extended periods of continuous monitoring.
Reference: Wanchaitanawong, J., Cotton-Clay, A., Baron, S., Fava, L., Easwar, V., Kinsolving, A., Zitser J., Leng, Y., Kahn, P., & Kushida, C. (2025)
Stanford validated and Peer-Reviewed
Read the entire publication at Science Direct:
https://www.sciencedirect.com/science/article/abs/pii/S1389945725004836
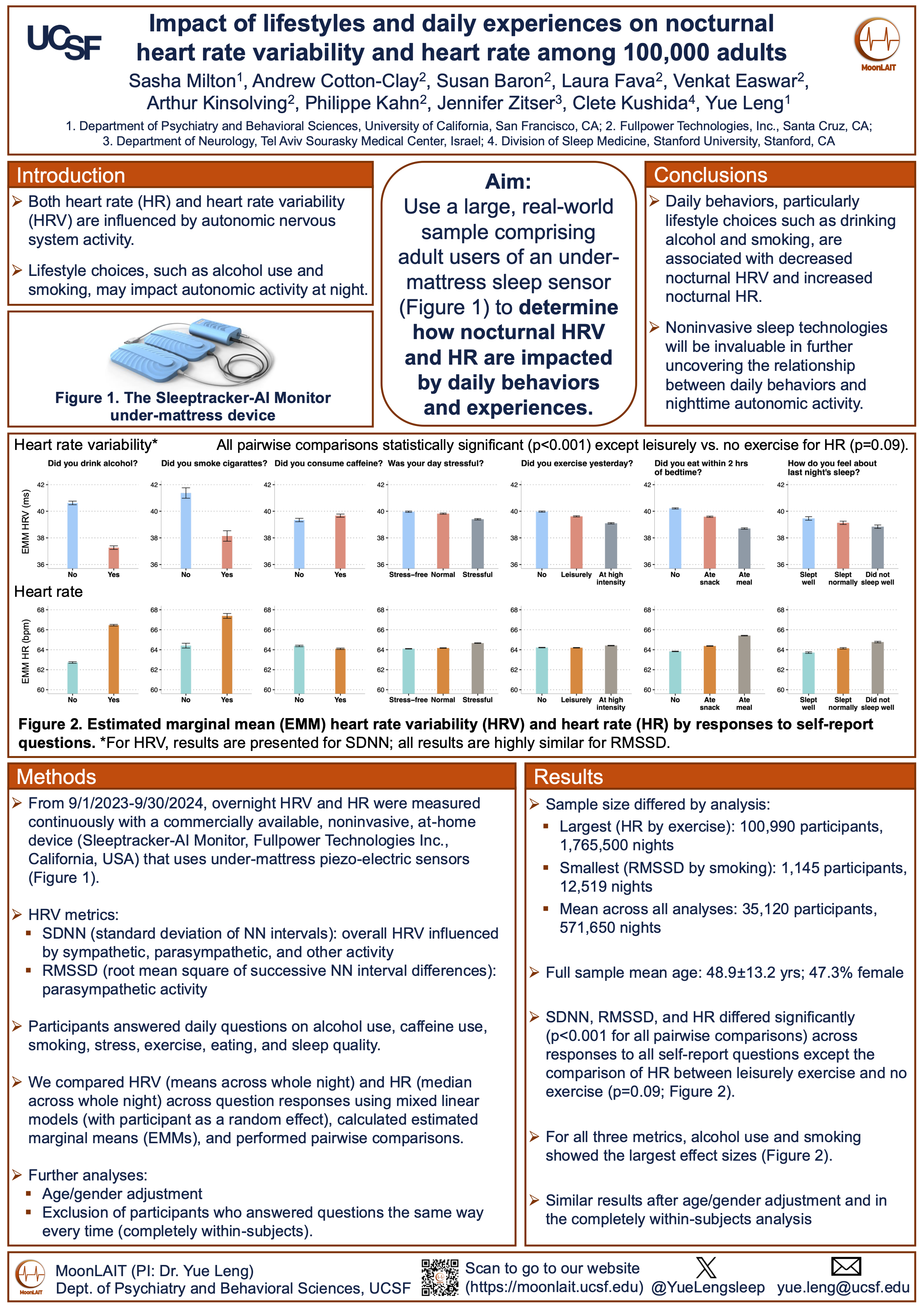
Impact of lifestyles and daily experiences on nocturnal heart rate variability and heart rate among 100,000 adults
 Click for PDF
Click for PDF
Both heart rate (HR) and heart rate variability (HRV) are influenced by autonomic nervous system activity. Lifestyle choices, such as alcohol use and smoking, may impact autonomic activity at night. Daily behaviors, particularly lifestyle choices such as drinking alcohol and smoking, are associated with decreased nocturnal HRV and increased nocturnal HR. Noninvasive sleep technologies will be invaluable in further uncovering the relationship between daily behaviors and nighttime autonomic activity.
Reference: Sasha Milton1, Andrew Cotton-Clay2, Susan Baron2, Laura Fava2, Venkat Easwar2, Arthur Kinsolving2, Philippe Kahn2, Jennifer Zitser3, Clete Kushida4, Yue Leng1
- Department of Psychiatry and Behavioral Sciences, University of California, San Francisco, CA
- Fullpower Technologies, Inc., Santa Cruz, CA
- Department of Neurology, Tel Aviv Sourasky Medical Center, Israel
- Division of Sleep Medicine, Stanford University, Stanford, CA
Validation of an Under-Mattress Monitoring Device Against Polysomnography for Heart Rate (HR) and Heart Rate Variability (HRV) Accuracy Assessment
 Click for PDF
Click for PDF
HRV is a key marker for autonomic nervous system function and sleep health. PSG with ECG is the gold standard but is complex for routine/home use. Advances in artificial intelligence have enabled the development of contactless, non-invasive sleep monitoring devices. The Sleeptracker-AI device from Fullpower uses multiple piezoelectric sensors placed under the mattress to detect heartbeats, respiration, and movement via ballistocardiography (BCG)
These findings indicate that the Sleeptracker-AI system provides reliable, long-term HR and HRV monitoring, particularly when beat detection coverage is high. Its non-invasive, contactless design makes it a practical tool for tracking cardiac autonomic dynamics and sleep health in real-world settings. Sleeptracker-AI supports its utility for both research and clinical applications.
E. Adibi1, A. Cotton-Clay2, A. Wray2, V. Easwar2, A. Kinsolving2, P. Kahn2, C. Kushida3, A. Hekmat3
- Prime West Consortium, Division of Internal Medicine, Redding, United States
- Fullpower Technologies, Inc. Santa Cruz, California, USA
- Stanford University, Division of Sleep Medicine, Palo Alto, United States
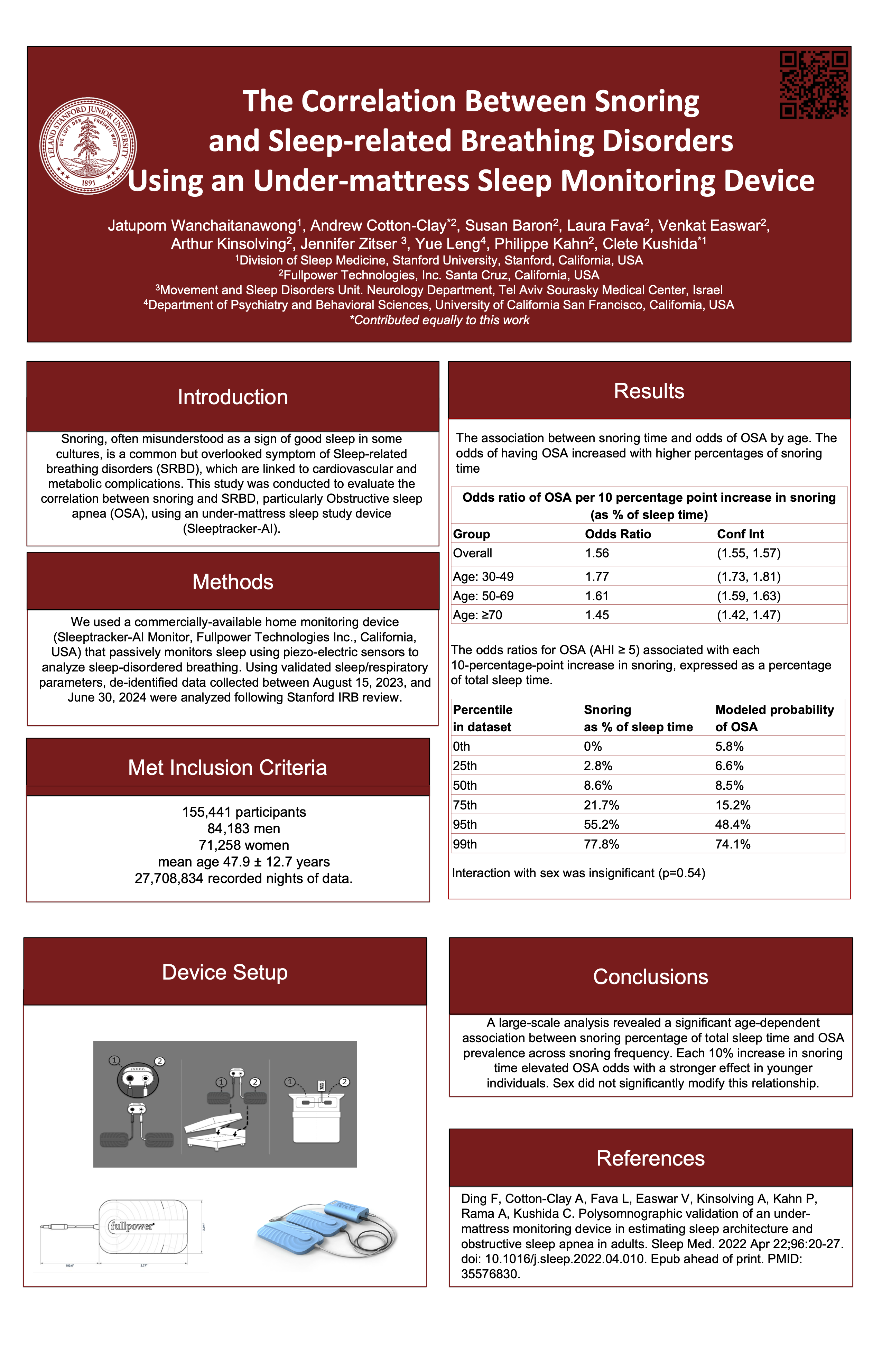
The Correlation Between Snoring and Sleep-related Breathing Disorders Using an Under-mattress Sleep Monitoring Device
 Click for PDF
Click for PDF
Snoring, often misunderstood as a sign of good sleep in some cultures, is a common but overlooked symptom of Sleep-related breathing disorders (SRBD), which are linked to cardiovascular and metabolic complications. This study was conducted to evaluate the correlation between snoring and SRBD, particularly Obstructive sleep apnea (OSA), using an under-mattress sleep study device (Sleeptracker-AI).
A large-scale analysis revealed a significant age-dependent association between snoring percentage of total sleep time and OSA prevalence across snoring frequency. Each 10% increase in snoring time elevated OSA odds with a stronger effect in younger individuals. Sex did not significantly modify this relationship.
Jatuporn Wanchaitanawong1, Andrew Cotton-Clay*2, Susan Baron2, Laura Fava2, Venkat Easwar2, Arthur Kinsolving2, Jennifer Zitser 3, Yue Leng4, Philippe Kahn2, Clete Kushida*1
- Division of Sleep Medicine, Stanford University, Stanford, California, USA
- Fullpower Technologies, Inc. Santa Cruz, California, USA
- Movement and Sleep Disorders Unit. Neurology Department, Tel Aviv Sourasky Medical Center, Israel
- Department of Psychiatry and Behavioral Sciences, University of California San Francisco, California, USA
*Contributed equally to this work