Over 200,000 New Daily Live Home Sleep Recordings With 5-Years Of History & 250+ Million Nights Of Sleep, Including Two Sleepers
Recorded with high fidelity, analyzed, and processed by our sleep experts using AI and machine learning; our tools analyze differences and changes over time in detailed sleep patterns day-after-day and includes the impact of two sleepers with one another.Monitor, Analyze, Share!
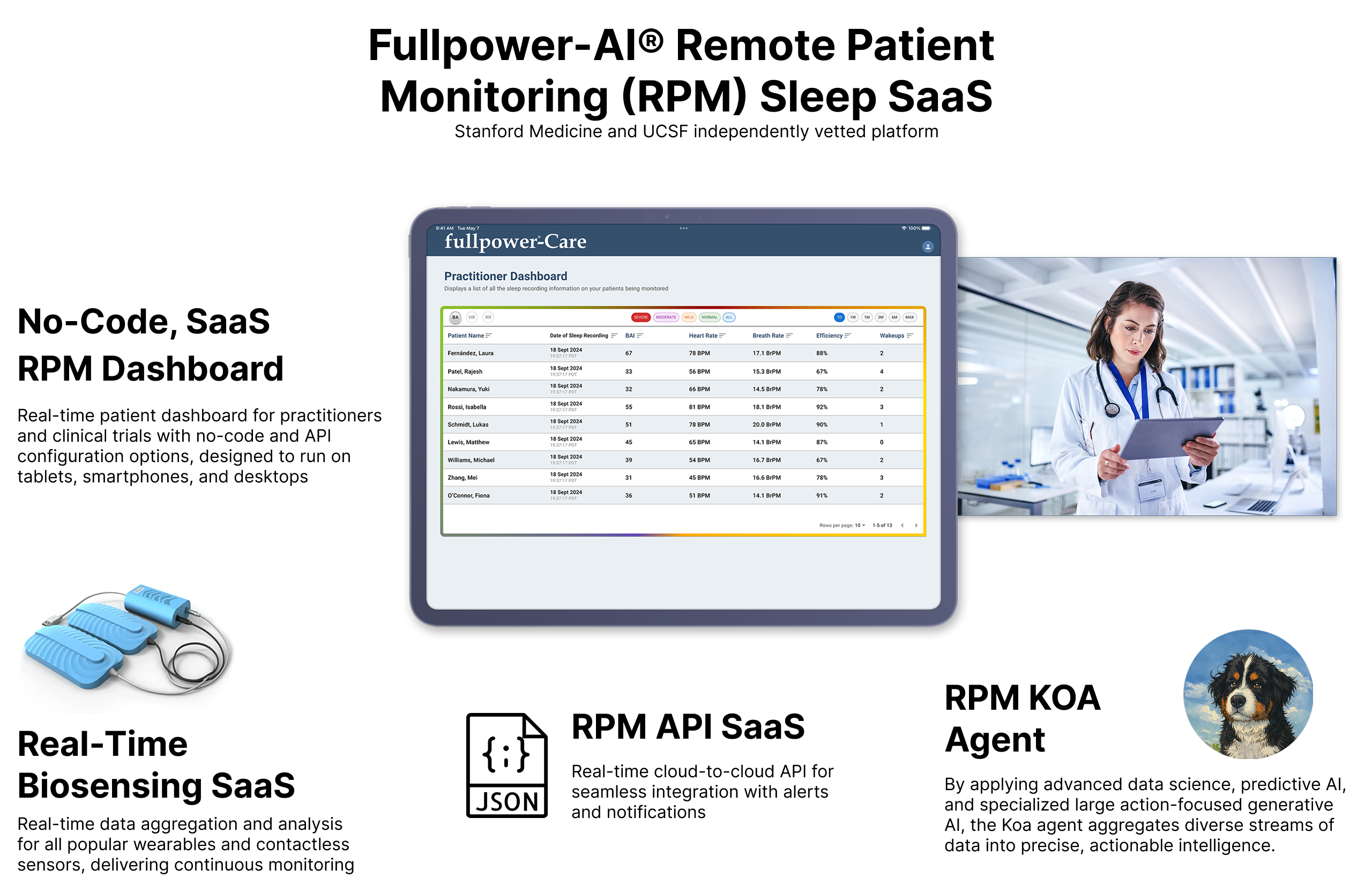
The Clinically Validated SaaS Platform
for Sleep Medicine, RPM, and Clinical Trials
250+ Million
Nights of High-Fidelity Sleep Data
30+ Parameters Monitored
Including BR, AHI, Arousal Index, HR, HRV, AQ, etc.
Stanford + UCSF
Validation & Collaboration
200K+
New Nights of Sleep / Day
15+
Countries
70+
Research Studies
10+
Publications
50+
Scientists & Technologists
Polysomnography
Labeling & Validation
Sensing is Real-time, contactless, & non-invasive monitoring
Dataset Access: Real-Time API and No-Code RPM Dashboard
Fullpower-AI's KOA LAM is setting a new benchmark for real-world health intelligence, transforming how we understand and manage health—anytime, anywhere.
Why KOA LAM?
1. Real-World Data
- Unmatched Scale: Built on 2+ billion biosensing datapoints from users in 140+ countries—and growing daily.
- Comprehensive Analysis: Pairs physiology (heart rate, breathing, motion) with environmental context (temperature, air quality, humidity).
- IoT Management: Orchestrates fleets of commercial biosensors with zero-touch management.
2. Clinically Validated by Leading Experts
- Trusted Accuracy: KOA LAM's insights are clinically validated by top institutions, including Stanford Medicine and UCSF.
- Global Recognition: Findings presented at SLEEP 2024, Sleep Europe 2024, and other international forums.
- Science-Backed Credibility: Trusted daily by physicians and research teams worldwide.
3. Real-Time Intelligence
- Sense-and-Response: Detects physiological events in real-time and triggers personalized responses.
- Continuous Monitoring: Tracks long-term trends critical to cognitive, metabolic, and cardiovascular health.
4. Transforming Medicine & Biosensing
- Continuous, Non-Invasive biosensing: Moves beyond the lab—scaling science into daily life enabling preventative medicine and next-generation research.
- Actionable Insights: Supports longevity, preventive care, and early intervention.
Partner with Fullpower-AI
Bring KOA's real-time biosensing intelligence to your patients, customers, or team. Let's build the next generation of health together.
Example of practical KOA LAM implementation
in sleep science and smart beds:
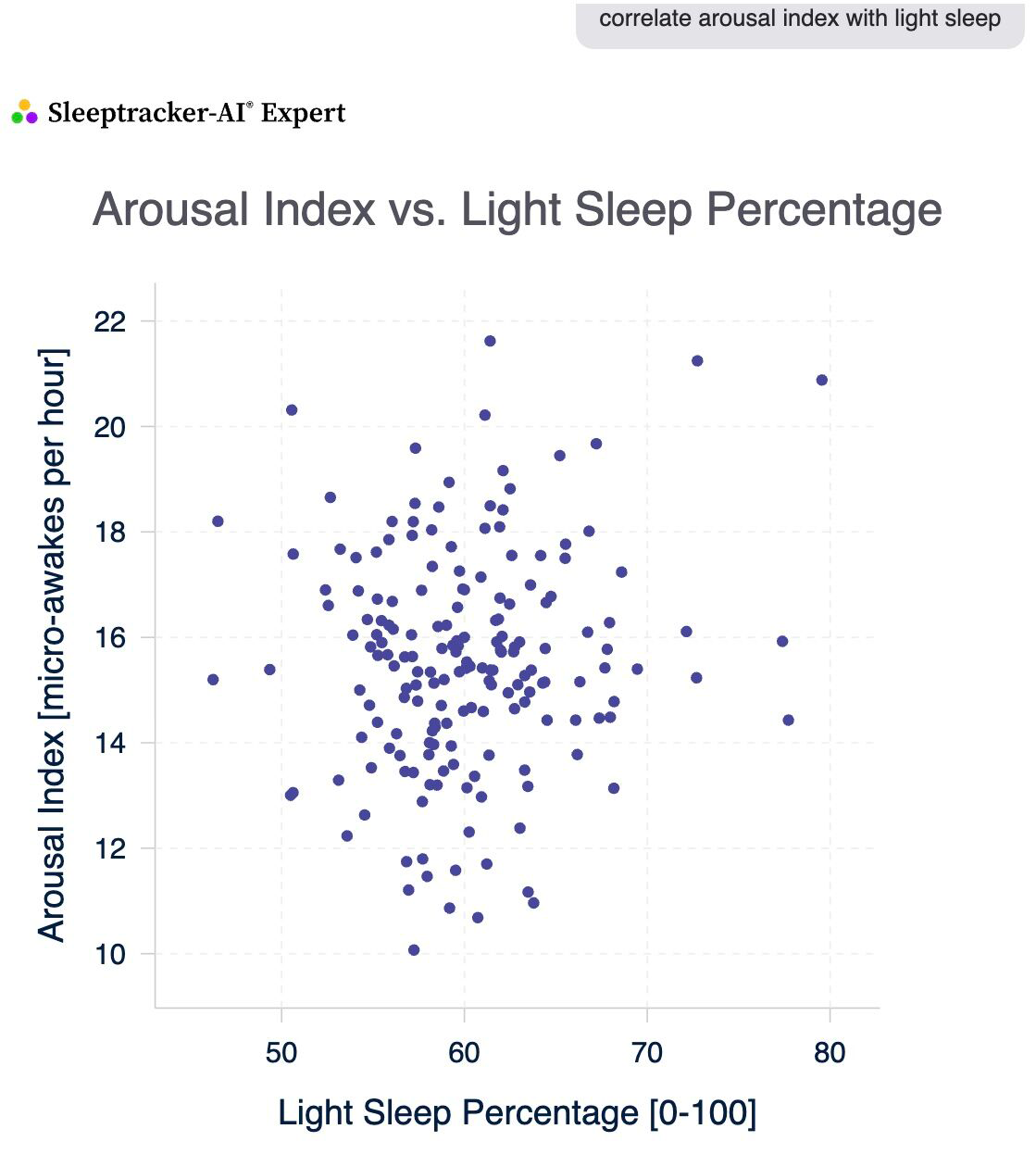
Arousal Index & Light Sleep: The Subtle Connection
-
There's a weak positive correlation between your arousal index (micro-awakes per hour) and light sleep minutes.
- When your light sleep is higher, your arousal index tends to be slightly higher too.
- For Example, with high light sleep, your arousal index averages around 16; with low light sleep, it's about 15.
- This means more light sleep might come with a few more micro-awakenings, but the effect is minor.
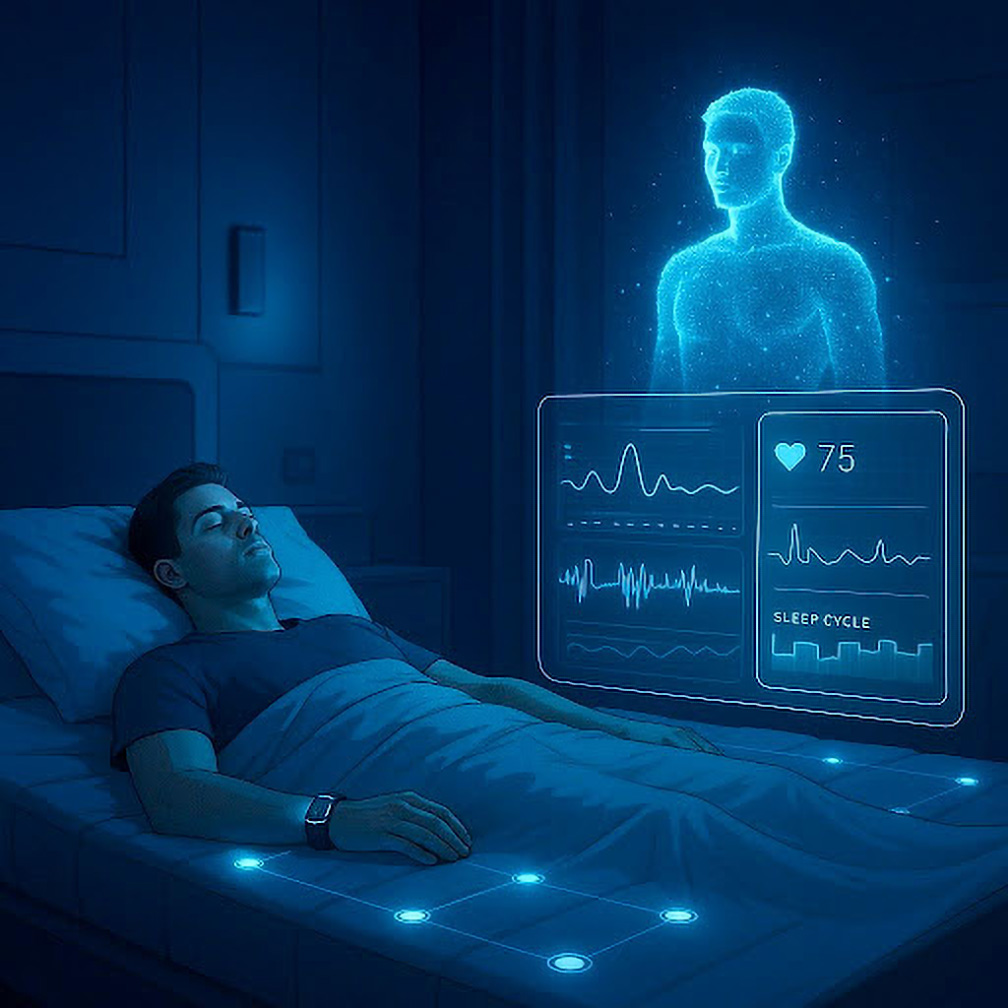
Empowering Health Through Digital Twins: Real-Time Biosensing for Optimized Sleep and Health
At the forefront of digital transformation, Fullpower-AI has long demonstrated clear leadership in the development and deployment of digital twin technology—well before the concept became widely recognized across industries.
Our patented innovations leverage real-time biosensing to create dynamic digital replicas of users and their environments, advancing health and wellness far beyond traditional passive monitoring. By integrating advanced sensors, intelligent algorithms, and adaptive sleep systems, our digital twins not only track and analyze vital health metrics but also proactively optimize conditions for rest, recovery, and performance.
From personalized sleep optimization to continuous, real-time modeling of daily behavior and environment, Fullpower-AI’s pioneering work has set the industry standard. As digital twin ecosystems continue to reshape our world, we are proud to empower individuals with actionable insights and intelligent automation—making every day healthier and more productive.
The Fullpower-AI KOA Digital Twin Platform provides a data-driven, real-time virtual model of individual physiological and behavioral states, integrating high-fidelity biosensing and artificial intelligence to advance precision health and wellness management.
Scientific Principles of the Fullpower-AI KOA Digital Twin Platform
Continuous Data Integration: The platform collects and fuses real-time data streams from a comprehensive array of wearables and biosensors, allowing for a multidimensional assessment of physiological parameters, including sleep, activity, and vital signs.Personalized Simulation and Prediction: Using advanced machine learning algorithms, Fullpower-AI's digital twins generate individualized predictions to inform proactive health interventions, risk stratification, and treatment optimization.
Dynamic, Adaptive Modeling: The digital twin adapts in real time as patient data updates, improving the accuracy of outcome modeling and enabling rapid adjustment of recommendations and care pathways.
No-Code and API Flexibility: Researchers and clinicians can implement models and adjust system parameters through user-friendly no-code interfaces or integrate with external systems using robust APIs for custom analytic pipelines and studies.
Applications in Medicine, Health, and Wellness
Patient Monitoring: Enables continuous, remote assessment of health status, supporting early detection of adverse events and chronic disease management.
Intervention Optimization: Simulates outcomes of lifestyle or therapeutic interventions, facilitating evidence-based personalization of treatment and preventive care plans.
Data-Driven Research: Aggregated, anonymized digital twin data supports large-scale studies on sleep, recovery, and wellness, contributing to new insights in precision medicine and public health.
By combining real-time biosensing, AI-driven prediction, and adaptive modeling, the Fullpower-AI KOA Digital Twin Platform advances the scientific foundation for personalized, preventive, and participatory health and wellness care.
Accuracy driven by deep learning and clinical validation. Here's how it works:
The Sleeptracker-AI® platform leverages deep learning to analyze anonymous sleep and environmental data.
- The Sleeptracker-AI® system determines sleep stages, aids in identifying sleep disorders, and provides users and clinicians with science-based sleep recommendations.
- We include a clinician/research no-code dashboard with triggers and event alerts for real-time notifications.
- Our accuracy closely matches gold-standard FDA-cleared PSG sleep analysis in real-world settings, as validated by Stanford Sleep Medicine. Our methodologies include deep, supervised, self-supervised, and reinforcement learning.
- We carefully consider ethical issues, bias, and privacy in our process. We operate multiple clinical PSG sleep labs to generate training data continually.
- We specialize in continuous care and clinical trials, and as noted, Stanford Sleep Medicine validates the accuracy of our system.
- We correlate sleep with environmental data automatically.
The Sleeptracker-AI SaaS platform provides valuable insights and tools for clinical trials, scientific research, and benefits a wide range of healthcare practitioners.

The Sleeptracker-AI SaaS platform developed by Fullpower-AI provides contactless remote in-home sleep monitoring for patients and real-time analytics with detailed no-code dashboard tools for clinical trials and practitioners. It also provides a real-time API for cloud-to-cloud integration.
Stanford Sleep Medicine and UCSF have vetted the system, ensuring high accuracy comparable to gold-standard polysomnography. The Sleeptracker-AI platform enhances patient care by offering the following benefits:
Completely noninvasive and contactless
There is nothing to wear or charge. It is invisible under any mattress and integrates environmental sensing to monitor breathing air quality and correlate it to sleep.
Early detection of issues
Remote monitoring with Sleeptracker-AI allows practitioners to identify sleep patterns or breathing disturbances before symptoms worsen.
Continuous monitoring
Sleeptracker-AI provides real-time and long-term data, offering a more comprehensive understanding of the patient's condition than periodic in-person visits and a retrospective perspective.
Improved treatment adjustments
Practitioners can adjust treatment plans based on continuous data from Sleeptracker-AI, changing medications, devices, or therapies as needed, improving patient outcomes.
Convenience for patients
Sleeptracker-AI eliminates the need for frequent in-person visits, which can be time-consuming or difficult for patients with mobility issues or living in remote locations.
Enhanced patient compliance
Patients are more likely to comply with prescribed treatments and follow up on care when they know their condition is continuously monitored.
Data-driven insights
Sleeptracker-AI provides practitioners with objective data, reducing reliance on subjective patient reports and enabling more accurate diagnosis and treatment.
Timely intervention
Practitioners can intervene promptly if critical signs, such as severe sleep disturbance episodes, are detected.
Cost-effective
Sleeptracker-AI reduces healthcare costs by minimizing the need for overnight sleep studies or hospital stays for monitoring purposes.
Patient empowerment
Patients can actively participate in their care by viewing their data and understanding their condition, leading to better engagement and lifestyle changes.
Expert deployment: Anil Rama, MD, a board-certified sleep physician, is deploying this new service at "Sleep and Brain, Powered by Sleeptracker-AI," ensuring expert care and oversight.
Integrations
Including Apple Health, Apple Watch, Pixel Watches, Samsung Watches, and Android Health Connect.


Case Study: COPD Care With Real-Time Response
Visit AnsibleHeath and Fullpower-AI® for information on this partnership.
Sleeptracker-AI: The Perfect Complement For Wearables
Clinically Validated
The Sleeptracker-AI® SaaS platform is validated in clinical studies with Stanford University, Division of Sleep Medicine, and UCSF


Clinical Trials and Research
Sleep is one-third of patients' lives and an important component in clinical trials and research
Polysomnographic validation of the Sleeptracker-AI® solution in estimating sleep architecture and obstructive sleep apnea in adults, in collaboration with Stanford Sleep Medicine, as presented by Dr. Clete Kushida at the 2022 Sleep World Congress in Rome (Italy).
Featured in Sleep Medicine
Volume 96, August 2022, Pages 20-27
Highlights
- An under-mattress sleep monitoring device (Sleeptracker-AI Monitor) was compared with polysomnography (PSG).
- Sleeptracker-AI Monitor estimated comparable sleep measures and had high agreement in sleep stage classification with PSG.
- Sleeptracker-AI Monitor had high accuracy in estimating obstructive sleep apnea.
Reference: Ding, F., Cotton-Clay, A., Fava, L., Easwar, V., Kinsolving, A., Kahn, P., Rama, A., & Kushida, C. (2022). Polysomnographic validation of an under-mattress monitoring device in estimating sleep architecture and obstructive sleep apnea in adults.Sleep medicine, 96, 20-27.
Stanford validated and Peer-Reviewed
Read the entire publication at Science Direct:
https://www.sciencedirect.com/science/article/pii/S1389945722001368
Estimated Sleep-Wake Patterns Obtained From a Large U.S. Sample Using a Home-Based Under-Mattress Sleep-Monitoring Device

Featured in the Journal of Sleep Medicine
Volume 21(3), December 31, 2024
Highlights
- Recordings were obtained using an under-mattress sleep monitoring device (Sleeptracker-AI Monitor).
- Sleeptracker-AI Monitor estimated comparable sleep measures and had high agreement in sleep stage classification with PSG.
Obstructive Sleep Apnea Detection and Prevalence in Men and Women Using a Continuous Large U.S. Sample by Home Under-Mattress Devices
Featured in
Sleep Medicine Online, September 16 2025
Highlights
- The prevalence of OSA is influenced by gender and age.
- Single-night sleep study may inaccurately classify OSA severity due to night-to-night variation.
- Home-based continuous sleep monitoring devices have the potential to enhance OSA diagnosis and address night-to-night variability.
- Sleeptracker-AI Monitor exhibits high sensitivity and specificity in diagnosing OSA during extended periods of continuous monitoring.
Reference: Wanchaitanawong, J., Cotton-Clay, A., Baron, S., Fava, L., Easwar, V., Kinsolving, A., Zitser J., Leng, Y., Kahn, P., & Kushida, C. (2025)
Stanford validated and Peer-Reviewed
Read the entire publication at Science Direct:
https://www.sciencedirect.com/science/article/abs/pii/S1389945725004836

70+ Very Large Dataset Sleep Studies Powered by ML and AI Analytics
Real-Time No-Code Dashboard Tools
Remotely monitor in real-time patients or all trial subjects with event alerts and notifications. This includes remote real-time vital signs, respiratory events, and sleep patterns of patients.Complete Integrated Machine Learning Modeling Tools With a Complete Set of AI-powered Analytical Tools
Supports supervised and unsupervised learning, deep-analysis, and infographics with statistical backing.AI-powered, Highly Accurate
Exceeds 90% accuracy of gold-standard Polysomnography in many key metrics. Large anonymized dataset of demographically diverse subjects ideal for use as a statistical reference to back trials and remote monitoring.135+ Patents, 10+ Years Of Sleep-Science And AI Leadership
Spanning AI, Machine Learning, Biosensing, Health, Cognitive Behavioral Science, Sleep Science, and more.Two Sleepers With Correlations in Real-Time
The data shows that two out of three beds have two sleepers. For the first time, two sleepers can be monitored and correlated to measure some of the effects of one sleeper on the other and build meaningful models.Built-in Environmental Sensing with Sleep Quality Correlations
The data shows that the room environment, including air temperature, air quality, and humidity, correlates to sleep quality.How the 9/22/25 Berkeley Earthquake Impacted Sleep Patterns
At Fullpower-AI, we’ve been reflecting on how the recent Equinox Berkeley earthquake affected our community in the Bay Area. The quake struck in the middle of the night, and with our KOA-powered Sleeptracker-AI platform, we saw just how many people’s sleep was disrupted in real-time.
Our graphical analysis shows patterns of waking and restless sleep across the region, but behind every data point is someone who was startled awake, checked in on loved ones, or tried to fall back asleep in the early hours.
If you were in the Bay Area during the quake, did it wake you up? How did you get back to sleep, and how did you feel the next day? We’d love to hear your experiences.
Debunking the sleep myth during the holidays. Hint: disruption!
Most of the data about Holiday sleep disruptions is based on surveys, more perception than objective data. For the first time, an objective multi-year study of more than 1 million nights of sleep compares the two weeks containing Christmas and New Year's to the first two weeks of December. This Sleeptracker.ai study shows how the season impacts our sleep patterns, often leading to sleep loss and disrupted routines. Here's a comprehensive look at how the holidays affect our sleep and what we can do to maintain healthy sleep habits during this festive time.

Impact of Holidays on Sleep: On average, people spend 6.6% more time awake in the middle of the night over the December holidays than normal. This sleep disruption is even more pronounced on New Year's Eve, with individuals spending 8.2% more time awake in the middle of the night than normal. We also see the highest average heart rate of the year, a full 2.2 bpm higher than earlier in the month.
Reasons for Sleep Disruption: Several factors contribute to holiday-related sleep issues.
Altered Eating and Drinking Habits: There is a 19% increase in adults reporting alcohol usage during the holidays, which can lead to poor sleep quality.
Less Exercise: There is a 6% decrease in adults reporting exercising, including an 11% decrease in reports of intense exercise, losing the benefits of exercise on sleep
Busier Schedules: Holiday events, late-night gift wrapping, and travel can disrupt regular sleep routines
Changes in Environment: Sleeping in unfamiliar places like hotels or guest rooms can affect sleep quality.
Tips for Better Sleep During the Holidays:
- Maintain a Consistent Sleep Schedule. Try to go to bed and wake up at the same time each day, even during the holidays. This consistency helps regulate your body's internal clock.
- Create a Relaxing Sleep Environment.
- Keep your bedroom cool (between 60-68°F), dark, and quiet.
- Use your bedroom primarily for sleep to maintain a strong sleep association.
- Mind Your Diet
- Limit caffeine intake, especially in the evening.
- Avoid heavy meals close to bedtime.
- If you choose to drink alcohol, do so earlier in the day and stay hydrated.
- Prioritize Physical Activity.
- Get outside for fresh air and natural light daily.
- Practice relaxation techniques like deep breathing or journaling before bed. Use the 4-2-4-2 breathing rule: Inhale for 4 seconds, hold for 2, exhale for 4, hold for 2, or some other popular technique.
By implementing these strategies, you can ensure you get the rest you need during the holiday season. This will allow you to enjoy the festivities while maintaining your health and well-being.
Thanksgiving Sleep Myth Debunked: Turkey's Not the Culprit!

Our study of 1M+ sleep nights shows that Thanksgiving ranks with Super Bowl Sunday and New Year’s Eve for poor sleep quality. Despite popular belief, turkey's tryptophan isn't to blame. Turkey doesn't contain significantly more tryptophan than other foods. This amino acid converts to serotonin and melatonin, two chemicals associated with sleep regulation. But turkey doesn't have substantially more tryptophan than other common foods like chicken, beef, nuts, or cheese.
Real sleep disruptors:
-Overeating
-Carb-heavy sides
-Holiday Stress
-Alcohol
For better sleep:
-Moderate portions
-Balance your plate
-Manage stress
Enjoy dinner and wake up refreshed on Friday!
Election 2024: How It Impacted America's Sleep
Our groundbreaking study at sleeptracker.ai reveals fascinating insights into how the 2024 election affected sleep patterns nationwide.
Key findings from our analysis of 1.6+ million nights of sleep:
• Significantly shorter sleep duration on election night as expected.
• Later bedtimes compared to typical weekdays as expected.
• Significantly higher heart rates during election night during sleep!
• Lingering effects from the recent Daylight Saving Time change, yet significant deepening of the sleep deficit.
What makes this study unique?
• 140,000+ sleepers tracked daily
• Clinically validated sleeptracker.ai platform and dataset with Stanford Sleep Medicine
• Real-time dataset analysis
We've created an eye-opening infographic to visualize these trends. Check it out!
How did the election impact YOUR sleep? Visit our LinkedIn thread to share your experience.
News
When Sleep Data Detects What Symptoms Don’t — A Landmark NEJM Case
Fullpower-AI December 02, 2025New Koa Research Sleep-Science Agent! Halloween as a Case Study
Fullpower-AI November 25, 2025Want More Deep Sleep? Live with a Dog or Cat!
Fullpower-AI November 11, 2025Daylight Saving Time (DST) creates a significant disruption in sleep schedules
Fullpower-AI November 02, 2025Empowering Health Through Digital Twins: Real-Time Biosensing for Optimized Sleep and Health
October 10, 2025How the 9/22/25 Berkeley Earthquake Impacted Sleep Patterns
September 23, 2025New Publication Announcement in Partnership with Stanford Sleep Medicine and UCSF
September 18, 2025Three New Sleep Science studies presented at World Sleep Congress 2025
Fullpower-AI September 11, 2025Somnigroup’s Strategic Bet on Sleep AI: A Pathway to Industry Leadership and Shareholder Value
AInvest August 09, 2025
Our mission is to make advanced AI biosensing universally accessible, empowering better sleep, Remote Patient Monitoring (RPM), and healthspan through real-time, science-validated intelligence.
Fullpower-AI is the developer of the Sleeptracker-AI platform
Our mission is to make advanced AI biosensing universally accessible, empowering better sleep, Remote Patient Monitoring (RPM), and healthspan through real-time, science-validated intelligence.
Visit Fullpower-AI